Plantar fasciitis, a common foot ailment affecting millions worldwide, brings discomfort and challenges to those who experience it. In this comprehensive article, we’ll delve into the intricacies of plantar fasciitis, examining its causes, symptoms, and exploring effective strategies for management and relief.
What is Plantar Fasciitis?
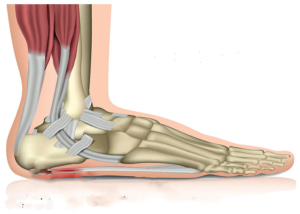
Anatomy of the Foot:
Before delving into plantar fasciitis, it’s essential to understand the foot’s anatomy. The plantar fascia, a thick band of tissue connecting the heel bone to the toes, plays a crucial role in supporting the arch of the foot.
Defining:
Plantar fasciitis is characterized by inflammation of the plantar fascia, resulting in heel pain. This condition often manifests as stabbing sensations near the heel, particularly during the first steps after waking or prolonged periods of rest.
Causes:
Excessive Strain and Overuse:
Plantar fasciitis often occurs due to excessive strain on the ligament, commonly seen in individuals who engage in activities that involve prolonged standing, walking, or running.
Foot Anatomy and Biomechanics:
Abnormal foot mechanics, such as high arches or flat feet, can contribute to plantar fasciitis. These variations alter the distribution of weight and impact how the plantar fascia absorbs stress.
Footwear and Lifestyle Factors:
Wearing unsupportive footwear or sudden lifestyle changes, such as increased physical activity, can trigger plantar fasciitis. Understanding these factors aids in prevention and effective management.
Symptoms of Plantar?
Plantar fasciitis is characterized by inflammation of the plantar fascia, the thick band of tissue that connects the heel bone to the toes. The condition commonly presents with the following symptoms:
- Heel Pain:
-
-
- The hallmark symptom is pain at the bottom of the heel, typically near the front and center of the heel pad. This pain is often most pronounced with the first steps in the morning or after periods of rest.
-
- Arch Pain:
-
-
- Discomfort or pain may also be felt along the arch of the foot, as the plantar fascia extends from the heel to the ball of the foot.
-
- Stiffness:
-
-
- Stiffness in the foot, especially after prolonged periods of inactivity, can be a symptom of plantar fasciitis.
-
- Discomfort While Walking:
-
-
- Individuals with plantar fasciitis may experience discomfort or pain while walking, particularly during the initial steps or after standing for an extended period.
-
- Radiating Pain:
-
- In some cases, the pain from plantar fasciitis may radiate along the sole of the foot, affecting mobility and the overall quality of life.
How can I prevent Diagnosis?
To prevent Plantar Fasciitis, incorporate these strategies:
- Proper Footwear: Choose shoes with adequate arch support and cushioning.
- Gradual Exercise: Increase activity intensity gradually to allow feet to adapt.
- Weight Management: Maintain a healthy weight to reduce stress on the plantar fascia.
- Stretching Routine: Regularly stretch calf muscles and the plantar fascia.
- Foot Care: Avoid walking barefoot on hard surfaces and consider orthotic inserts.
- Balance Activities: Alternate high-impact activities with low-impact ones.
- Professional Guidance: Seek professional advice for customized preventive measures based on individual factors.
When to Contact a Medical Professional Exams and Test
If you experience persistent heel pain or suspect Fasciitis, consult a medical professional. They may conduct a clinical examination, assessing symptoms, foot mechanics, and lifestyle factors. In some cases, imaging studies like X-rays or ultrasounds may be recommended to rule out other causes and provide a comprehensive diagnosis. Timely medical evaluation ensures an accurate assessment and allows for the implementation of appropriate treatment measures tailored to your specific condition.
Surgery Stretching and Physical Therapy
Plantar fasciitis treatment typically involves non-surgical methods, with surgery considered only in severe cases resistant to conservative measures. Here’s an overview of common approaches:
- Stretching:
-
-
- Regular stretching exercises targeting the Achilles tendon and calf muscles help alleviate tension on the plantar fascia, promoting flexibility and reducing symptoms.
-
- Physical Therapy:
-
-
- Physical therapy sessions may address muscle imbalances, improve foot mechanics, and enhance overall foot strength and flexibility, contributing to the relief of plantar fasciitis.
-
- Surgery (in Severe Cases):
- Surgical intervention is considered when conservative treatments fail. Procedures may involve releasing the tension on the plantar fascia, removing heel spurs, or addressing other contributing factors. Surgical options are typically reserved for cases unresponsive to other treatments.
It’s essential to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan based on the severity and specific characteristics of your plantar fasciitis.
Conclusion:
Plantar fasciitis, while a challenging condition, is manageable with a comprehensive approach to treatment and prevention. By understanding the causes, recognizing symptoms, seeking timely medical evaluation, and adopting effective management strategies, individuals can navigate the path to relief and regain their mobility and comfort. Plantar fasciitis doesn’t have to be a constant source of pain; with the right interventions, individuals can step forward on a journey toward improved foot health and overall well-being.